Eclampsia: Understanding a Serious Pregnancy Complication
Eclampsia is a severe and potentially life-threatening complication of pregnancy, characterized by the onset of seizures in a woman with preeclampsia. Preeclampsia, a condition marked by high blood pressure and often protein in the urine, typically arises after 20 weeks of gestation. When preeclampsia progresses to eclampsia, it signifies a critical escalation that requires immediate medical attention to protect both the mother and the baby.
Understanding Eclampsia
Eclampsia, although relatively rare, remains a significant cause of maternal and fetal morbidity and mortality worldwide. It affects about 1 in 2000 to 1 in 3000 pregnancies in developed countries but is more common in developing regions due to disparities in prenatal care.
Symptoms and Signs
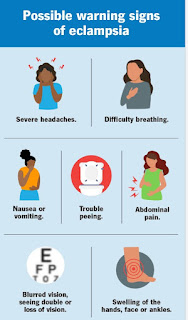
Eclampsia is primarily identified by the occurrence of seizures in a pregnant woman diagnosed with preeclampsia. However, other signs and symptoms often accompany this condition, including:
1. Severe Headaches: Persistent, throbbing headaches that do not subside with usual pain relief measures.
2. Visual Disturbances: Blurred vision, temporary loss of vision, light sensitivity, or seeing spots or flashes.
3. Upper Abdominal Pain: Pain in the upper right quadrant of the abdomen, indicative of liver involvement.
4. Nausea or Vomiting: Especially if it appears suddenly in the second half of pregnancy.
5. Altered Mental Status: Confusion, agitation, or changes in consciousness.
Causes and Risk Factors
The exact cause of eclampsia is not fully understood, but it is believed to involve abnormal development of the placenta, leading to issues with blood flow and a cascade of systemic complications. Several risk factors increase the likelihood of developing eclampsia:
1. History of Preeclampsia or Eclampsia: Previous pregnancies affected by these conditions.
2. Chronic Hypertension: High blood pressure existing before pregnancy.
3. Kidney Disease: Pre-existing renal conditions.
4. Diabetes: Both type 1 and type 2 diabetes.
5. Multiple Pregnancy: Carrying more than one fetus.
6. Obesity: High body mass index (BMI) before pregnancy.
7. Age: Younger than 20 or older than 35 years.
Diagnosis and Monitoring
Eclampsia is diagnosed primarily through clinical observation of seizures in a pregnant woman with preeclampsia. Monitoring involves regular prenatal visits where blood pressure is measured, and urine is tested for protein. Advanced diagnostic techniques include:
1. Blood Tests: To check for signs of hemolysis, elevated liver enzymes, and low platelet count (HELLP syndrome), which often accompanies severe preeclampsia and eclampsia.
2. Imaging: Ultrasound to monitor fetal growth and amniotic fluid levels.
3. Non-Stress Tests: To evaluate fetal well-being.
Treatment and Management
Immediate medical intervention is crucial in managing eclampsia. The primary goals are to control seizures, manage blood pressure, and expedite delivery if necessary. Key treatment strategies include:
1. Magnesium Sulfate: The drug of choice for preventing and controlling seizures.
2. Antihypertensive Medications: To manage high blood pressure.
3. Steroids: If delivery is imminent, to accelerate fetal lung maturity.
4. Delivery: Often the definitive treatment; the timing and method depend on the severity of the condition and the gestational age of the fetus.
Prevention and Prognosis
Preventing eclampsia involves early detection and management of preeclampsia. Regular prenatal care, including monitoring blood pressure and screening for proteinuria, is vital. For women at high risk, low-dose aspirin and calcium supplements may be recommended.
The prognosis for eclampsia can be favorable with prompt and effective treatment, but it remains a leading cause of maternal and neonatal morbidity and mortality in resource-limited settings. Long-term follow-up is essential, as women with a history of eclampsia have an increased risk of cardiovascular diseases later in life.
Conclusion
Eclampsia is a serious and life-threatening complication of pregnancy that demands swift medical intervention. Understanding its signs, risk factors, and treatment options is crucial for healthcare providers and expectant mothers alike. With vigilant prenatal care and timely management, the risks associated with eclampsia can be significantly reduced, ensuring better health outcomes for both mother and child.
Comments
Post a Comment